Together with the nursing and supporting staff, we offer in-patient se...
Read MoreHighly precise technique that allows delivery of high dose radiation t...
Read MoreTo treat tumors in chest, abdomen or pelvis that cannot be removed sur...
Read MoreExternal beam radiation therapy that can be completed in 1 to 5 treatm...
Read MoreAdvanced imaging modalities with in-room imaging facilities to adjust ...
Read MoreAdvanced radiotherapy technique which uses inverse planning and dose c...
Read MoreManagement of primary malignant bone tumors of the extremity has chang...
Read MoreAs part of conditioning regimens for acute leukemia and to deliver org...
Read More Overview
Overview The Department of Oncology at Amala Hospital started in 1978is one of the first cancer centres in Kerala. The Radiation Oncology department initiated its work with 3 cobalt teletherapy machines and later upgraded with 2 linear accelerators (UNIQUE in 2013 and TRUBEAM in 2023) and brachytherapy. The programs offered by the department are of international standards with advanced Clinical Radiation Therapy techniques and treatment. The department comprises of a dedicated team of doctors, highly trained and qualified medical physicists, radiation technologists, well trained oncology nurses, and supportive care team members. The department has been accredited by NABH, and it strives towards ensuring a patient-centred, cost-effective and high quality of comprehensive radiation treatment.
Linear Accelerators are used for external beam treatment of tumors. The Department has the latest Linear Accelerator Truebeam with HD120-MLC v2.7, state of the art, premium end, high dose rate, delta couch with 6 degrees of freedom movement. Installed in 2023, the first of its kind in Kerala, it uses Artificial intelligence incorporated treatment software which enhances treatment precision.
Installed in 2013, UNIQUE by the Varian allows us to perform various treatment techniques including 2D and 3D radiation therapy, IMRT and RapidArc.
Besides external radiation treatments, in-body treatments (Brachytherapy) are also performed. In our center, GAMMAMED PLUS HDR installed in 2012, in which in-body treatments are performed, is a brachytherapy device. Brachytherapy is used in the intra-cavity or intra-tissue radiation therapy of uterine, esophagus and bronchial tumors. The radio-active source Iridum-192, is placed in the space or tissue using applicators and treatment is delivered. Dose calculations are made in the ECLIPSE Treatment Planning system and then radioactive material is loaded from outside.
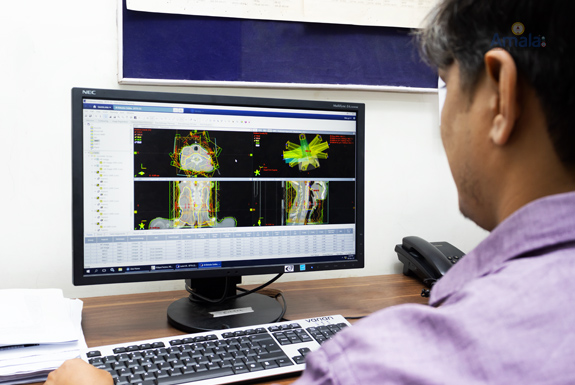
TPS comprises of computers and software programs which are the key to improved patient outcomes. Once image datasets are loaded and the tumors are identified, the systems develop a complex plan quickly and accurately on how the system will deliver radiation. The software computes the expected dose distribution in the patient’s tissue. These systems also help navigate beam placement based on avoiding critical structures. These tools are essential for precise treatment delivery.
CT simulators have become the standard of care for radiotherapy. Our department has the Optima CT 550, which is a 16 slice dedicated CT simulator. It is a real-time, CT-linked, 3-D treatment planning system, which consists of a CT scanner, a multi-image display, a treatment planning device with real-time visual optimization, and a laser beam projector.





The simulated set up being exactly reproduced before each treatment by matching the reference lasers in the treatment room to the tatoos and comparing 2D-3D OBI with the simulation C.T-Scan

High precision treatment being delivered under the supervision of the radiation Oncologist and Physicist.

True beam with HD 120 MLC V.2.7 State of the art Premium End high dose rate Radio surgery linear Accelerator with rapid arc and delta couch (perfect Pitch 6DoF) with AI incorporated treat

Brachytherapy unit

simulation being performed at the simulation room with a dedicated CT Scanner

Contours being delineated for treatment planning process that involves at outlining targets and organs at risk to guide RT plans that optimize tumor control & reduce radiation toxicity

CT Scan being performed to acquire the images to identify the lesions and surrounding normal clinical structures

High precision treatment being delivered under the supervision of the radiation Oncologist and Physicist.

True beam with HD 120 MLC V.2.7 State of the art Premium End high dose rate Radio surgery linear Accelerator with rapid arc and delta couch (perfect Pitch 6DoF) with AI incorporated treat

The simulated set up being exactly reproduced before each treatment by matching the reference lasers in the treatment room to the tatoos and comparing 2D-3D OBI with the simulation C.T-Sc

Contours being delineated for treatment planning process that involves at outlining targets and organs at risk to guide RT plans that optimize tumor control & reduce radiation toxicity

Post graduate teaching programme designed to prepare students for technical and theoretical and practical aspects of the field

High precision treatment being delivered under the supervision of the radiation Oncologist and Physicist.
The simulated set up being exactly reproduced before each treatment by matching the reference lasers in the treatment room to the tatoos and comparing 2D-3D OBI with the simulation C.T-Scan
Facilities are available on all working days (Monday – Saturday) from 8:00 am to 4:00 pm.
Day care chemotherapy.
Radiotherapy treatment and planning services on all working days (Monday – Friday) and on Saturdays in case of emergency.
Together with the nursing and supporting staff, we offer in-patient services to those who need intensive care during or after Radiation Therapy. Services are also provided to patients who wish for hospital stay during the course of treatment or those who require Chemotherapy.We also have 24x7 Oncology ICU service for those who need critical care with highly trained ICU nursing and supportive staff.
Highly precise technique that allows delivery of high dose radiation to conform to small tumors in a very short period of time.
Treats both benign and malignant brain and spine tumors.
To treat tumors in chest, abdomen or pelvis that cannot be removed surgically or treated with conventional Radiation Therapy.
It involves using very secure immobilization of the head or body as well as using techniques that allow the radiation beam to account for organ motion during treatment.
Our first SBRT to the Liver was successfully done in January 2023 .
External beam radiation therapy that can be completed in 1 to 5 treatments, with extreme accuracy, minimizing the effect on adjacent critical organs.
Suitable for small-well defined tumors.
Advanced imaging modalities with in-room imaging facilities to adjust for tumor motion or patient setup accuracy between treatments. This allows for more accurate delivery of radiation. We use 2D based kV and MV imaging or 3D based Cone Beam CT. This technique is used for prostate, lung, breast malignancies as well as SRS, SBRT.
Advanced radiotherapy technique which uses inverse planning and dose calculation while delivering highly conformal radiation. The radiation beam is broken up into many beamlets and the intensity of each beamlet can be adjusted individually. It safely allows a higher dose of radiation for improved tumor control with significant sparing of organs at risk.
Successful treatment outcome in radiation oncology is based on irradiation of tumor-bearing tissues to adequate, or curative doses; and the sparing of normal, or uninvolved, tissues from unnecessary radiation. The radiation beams can be precisely tailored to the size and shape of the tumor using MLCs.
Time-tested and reliable radiation technique; cost-effective.
Most often used for palliative intent Radiotherapy .
Management of primary malignant bone tumors of the extremity has changed dramatically over the last few decades. Amputation has been replaced by limb-conservation therapy. One approach for limb reconstruction is reimplantation of the tumor bearing bone following extracorporeal irradiation. Here the tumor bearing bone segment is resected, treated with a single fraction of radiation therapy extracorporeally and re-implanted with fixation devices. ECI is done in collaboration with the Department of Orthopaedics.
As part of conditioning regimens for acute leukemia and to deliver organ spared targeted Radiotherapy in those undergoing Hematopoietic cell transplantation
More targeted forms of Radiotherapy which have the potential to decrease toxicity and escalate the dose to the entire body bone marrow
Radio-active source (Iridium-192) is placed within the body cavity or tissue using applicators and radiation is delivered.
Brachytherapy is suggested for Endometrial Malignancies as day care procedure. The treatment takes about 5-15 minutes.
Brachytherapy for cervical malignancies are done under short GA, for whom IP services are provided. The treatment schedule which includes 3 applications is completed in 1 week time.
Majority of the cases dealt by the Radiation department at Amala IMS are Endometrial, Cervical and Vaginal Malignancies. Our physicians also have expertise in Endobronchial Brachytherapy.
PG Training
MD program was started in 2017. The department has an annual intake of one PG resident for the course of MD Radiation Oncology (duration 3 years). As per NMC regulations, patient-oriented course with experience in outpatient and inpatient care, planning and execution of treatment, Brachytherapy and chemotherapy training, is offered. Academic training sessions include Radiation Oncology lectures, Radiation Physics classes, regular journal clubs, case presentations and discussions. PGs are also posted in various departments such as Nuclear medicine, Radiology, Medical Oncology, Surgical Oncology, Pain and Palliative Care, ENT and Pathology.
UG Training
As per curriculum, UG residents are posted for a 1 week period during their 2nd year of MBBS and internship. They are offered training in basic knowledge in Oncology, along with OP and IP care. End posting exams, which include case presentations and discussions and role play are conducted on a regular basis.
DRT Training, M.SC. Oncology
Regular classes, hands on experience and training are provided on patient care, Radiotherapy treatment techniques, with regular exams being conducted.